Do Masks Prevent COVID-19?
Louis M. Katz MD and Cheryl True MD
Should masks be used in community settings (not health care) to prevent COVID-19? The question is important as we come into fall and winter when cold weather will drive people indoors and into crowded settings. Early advice not to use masks in public were driven by our lack of understanding of how often the virus was transmitted from people without symptoms and the need to save masks for frontline healthcare workers when supplies were short. People with no symptoms cause a large part of transmission and shortages are largely gone.
The best proof that masks work, controlled experiments, is not available, but the other evidence is convincing. Animal experiments and observational studies show that masking of both infected people and contacts greatly reduces transmission of SARS-CoV-2. This makes sense: they block the virus from getting out of an infected person and from getting into the airway of a contact. They may also reduce the severity of COVID-19 even when full protection fails (probably by reducing the amount of virus that establishes an infection). (Source)
Animal studies:
These can be well controlled and are very convincing.
Hamsters have been infected with SARS-CoV-2 and housed next to uninfected animals with their cages separated by either screens or mask material. If separated by mask material, they have less than half as many infections and those that are infected become less ill. (Source)
Observational studies:
These provide useful data but can be confusing when two or more interventions are used at the same time.
- Summer camps without mask mandates suffered explosive outbreaks. This is a bit confounded by congregate sleeping arrangements. (Source)
- Black Lives Matter demonstrations, where video evidence documents a high level of masking, have not been followed by infection spikes. Risk is also lowered by the outdoor venues involved. (Source)
- At the Sturgis motorcycle rally, there was little masking and no social distancing in crowded, poorly ventilated indoor venues (bars esp.). There were at least 290 cases of COVID-19 in attendees with a spike of cases in the community hosting the event. A study using cellphone GPS data and case counts has associated Sturgis with as many as 20% of US COVID-19 cases during August 2020 (this high-end estimate is controversial). (Source) The rally’s real impact is most probably somewhere between the two numbers but is clearly not trivial.
- In a study of data from 196 countries, mask-wearing by the public was independently associated with lower COVID-19 mortality. (Source)
- US states mandating mask use saw falls in the rate of epidemic growth compared to states with no mandates. This provided an estimate that masks were associated with 230,000-450,000 fewer cases of COVID-19 by May 22, 2020 (without considering enforcement procedures). (Source)
- Use of masks was studied in 124 households with a first case of COVID-19 and followed 355 contacts. Masking of contacts before the onset of symptoms in the first case decreased infection by 80%. Use of masks only after the onset of symptoms was not effective. This kind of evidence is important because households are a source of very intense exposure and a high risk of infection. (Source)
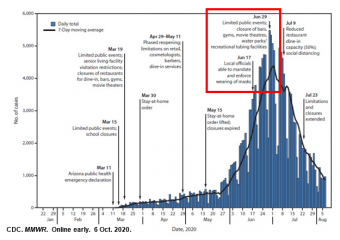
- In Arizona, cases and deaths spiked after the end of social distancing rules during May. In June, there was a rapid fall in new cases that began 12 days after cities were allowed to require and enforce mask use. This is exactly the interval after which a decline from the intervention would be expected. Other interventions may have contributed, but the time course really suggests that masks were the major contributor. (Source)
- Two hairstylists in Missouri were ill with COVID-19 but kept working during July. They had 139 close customer contacts over a two-week period during which both parties were masked. No transmission was documented. The stylists transmitted to their contacts outside the workplace when masks were absent. (Source)
- Modeling studies estimate that 95% mask use in the US between late August 2020 and New Year’s Day 2021 would prevent between 60,000 and 151,000 deaths. (Source)
What is coming:
Two large trials randomized experiments in humans should be available in the near future.
One in Denmark has been completed in which 6000 people were randomized to a request to use masks in workplace or not. The study is completed but no results are available.
A study is in progress in Guinea-Bissau with 40,000 people in households randomized to receiving masks or not. All will receive advice on how to protect themselves from COVID-19. The study is to be fully enrolled during November, with the participants followed for COVID infections for several months.
Bottom line:
Masks work to prevent COVID-19. The White House Coronavirus Task Force recommended a mask mandate in Iowa because of uncontrolled spread in the state. Masks are safe, simple, and cheap. (Source) Absent mandates, businesses are in a perfect position to require masks on their premises and individuals to model mask wearing as an expected pro-social behavior. Masks combined with scrupulous social distancing, hand hygiene and other recommended prevention measures are a critical part of COVID-19 prevention strategies.
Louis M. Katz MD and Cheryl True MD are the medical directors of the Scott and Rock Island Co. Health Departments, respectively. Their opinions to not necessarily reflect the official positions of either department.