Confused about COVID boosters? Here’s a quick, painless user’s guide for you

What you need to know about if, when and where to get a coronavirus vaccine booster in San Diego County.
Struggling to make sense of all the information swirling around coronavirus vaccine boosters? You’re not alone.
In recent weeks, federal and state officials have given the green light for broad swaths of the population to get boosters. But they’ve done so using language that’s not always clear and offers limited guidance on whether certain people should get the shots and which vaccine to get.
Here’s a quick rundown of what you need to know, with some perspective from local researchers.
Wait, who’s eligible for boosters again?
If you got your second dose of the Pfizer or Moderna vaccine at least six months ago and are 65 or older, you’re eligible. If you’re younger and got your last shot at least six months ago, you’re also eligible if you have health conditions that put you at higher risk of COVID-19 or if you live or work in a setting where you’re more likely to get infected. That includes people living in jails or homeless shelters, health care workers and those with liver disease, diabetes and other underlying conditions.
But here’s where those guidelines, outlined by the Centers for Disease Control and Prevention, get a bit complicated. The agency says that anyone 65 and up should get a booster if enough time has passed since their last shot, and it makes a similar recommendation for people 50 to 64 with underlying medical conditions. But the CDC simply says that younger people who are eligible may choose to get a booster.
Things are more clear-cut for Johnson & Johnson’s vaccine, as the CDC encourages anyone who got the one-shot vaccine two or more months ago to come back for seconds.
Why all the hedging, and why the difference between vaccines?
Part of the answer is that there’s ample evidence vaccines still prevent COVID-19 hospitalization and death among most people, though protection has dipped slightly among those who are older and sicker, says Dr. Mark Sawyer, infectious disease expert at Rady Children’s Hospital. Sawyer was part of the scientific advisory panels that recommended the Food and Drug Administration authorize all three vaccines, and he’s also voted in favor of the current booster rollout.
“People in the younger age groups, especially if they don’t have any underlying health conditions, are really at no significant risk,” he said. “If they’re concerned about COVID, sure, get a booster. If they’re not, or if they’re for some reason really concerned about side effects of the vaccine, then you don’t need to go run out and get a booster.”
That’s the same advice Sawyer has given to Rady’s pediatric medical residents, many of whom are in their 20s and 30s, and to one of his daughters, a health care worker in her mid-30s.
The authorization of Johnson & Johnson boosters regardless of age, health or occupation reflects data from numerous groups showing that a single dose of this vaccine isn’t as effective as the two-shot Moderna and Pfizer vaccines. A CDC study based on data from March to August found that the one-shot vaccine was about 70 percent protective against COVID-19 hospitalization, while the other vaccines were roughly 90 percent effective.
Many are seeking extra doses through local pharmacies and health systems, even though public health officials have yet to agree on a plan for rolling out booster shots.
Where can I get the shots?
For the most part, the same places you went to get immunized earlier this year or last: pharmacies, county-run sites and local health systems.
The booster rollout began slowly and unevenly across vaccine providers in late September. But now, UC San Diego Health, Kaiser Permanente and Sharp HealthCare are offering boosters of all three vaccines, according to spokespersons for these systems and information available on their websites. A Scripps Health spokesperson confirmed that they’re offering Moderna and Pfizer boosters. Many of these health systems are reaching out to patients to let them know they can come in for boosters, though you can also contact your provider.
Pharmacy chains such as CVS and Ralphs are asking that you schedule an appointment for a booster online rather than walk in. In the case of CVS, that’s because some stores only offer the Moderna vaccine, for which boosters have yet to be approved, while other locations offer Pfizer shots.
Mass public vaccine sites like the ones near Petco Park and the Del Mar Fairgrounds shut down earlier this year as the demand for doses dipped and as numerous smaller vaccine sites popped up. There are now more than 300 locations throughout the region where you can get immunized, according to county spokesperson Mike Workman.
You can use the state’s vaccine scheduling system, MyTurn (myturn.ca.gov), to check whether you’re eligible for a booster and find a vaccine site near you.
The rollout of Pfizer booster shots is proceeding slowly and unevenly across the region’s health care systems and pharmacies
What’s in these shots, and how do they “boost” immunity?
The contents of the booster shots are no different than the original vaccines. For Pfizer and Moderna, it’s an RNA molecule with genetic instructions that teach your body to recognize and attack the surface of the coronavirus. Johnson & Johnson uses a modified common cold virus to slip essentially those same instructions inside your cells, sparking an immune response.
Pfizer and Johnson & Johnson use the exact same dose of their initial vaccine as a booster, while Moderna uses a half-dose.
These shots fire up immune cells still around from the first time you were vaccinated, leading to stronger and longer-lasting protection. Most of the cells that respond to a vaccine or infection eventually die. But some stick around in case you’re ever exposed to the virus again, ready to launch a swift counterattack. These immune cells, known as memory cells, include T cells, which can kill infected cells, and B cells, which make antibodies, the Y-shaped proteins that can latch onto a virus to prevent infection.
A quick rundown of what antibodies can (and can’t) tell us about COVID-19
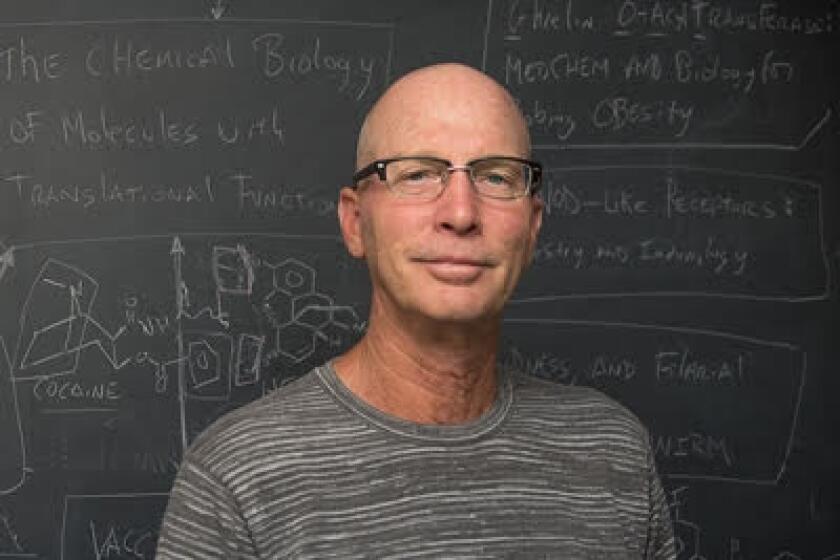
Shane Crotty, a researcher at La Jolla Institute for Immunology, says that he and colleagues have learned that COVID-19 vaccines trigger strong B and T cell memory responses. But the level of antibodies floating around in a person’s blood wanes with time. Studies from vaccine makers show that boosters bring those levels back up, and Crotty thinks an extra dose could ensure that they stay up for longer.
“That’s basically a cost-benefit analysis your immune system is running. It takes real calories and energy to make antibodies for years,” Crotty said. “It’ll probably happen after three doses, because, overall, the immune memory looks good to those vaccines.”
Can I mix and match vaccines?
You can, but the CDC hasn’t taken a position on the real question — should you?
“Some people may have a preference for the vaccine type that they originally received, and others may prefer to get a different booster. CDC’s recommendations now allow for this type of mix and match dosing for booster shots,” said the agency in an Oct. 21 statement.
It’s no accident the agency’s statement is vague. There’s limited data on mixing and matching coronavirus vaccines, as the companies that developed these shots have only tested boosters of their own vaccines.
But there is some evidence to suggest that mixing vaccines is safe and effective. That includes an ongoing study by the National Institutes of Health in which about 450 people either got a booster of the same vaccine they’d first gotten or a different brand. Notably, antibody levels in people who’d first gotten the Johnson & Johnson vaccine typically went up 33- or 56-fold if they got a Pfizer or Moderna booster, respectively, compared with a 4.6-fold antibody increase from a second Johnson & Johnson shot.
“If originally you got Moderna or Pfizer, getting a booster of either is fine. They’re going to be pretty much identical,” Crotty said. “For the J&J vaccine, it’s different,” he added. “If you’re looking at the immune responses, it seems pretty clear-cut that you’re better off mixing and matching there if you’re willing to do it.”
Other reports, including a U.K. study published in June, show that mixing and matching AstraZeneca’s vaccine with an RNA vaccine sparks stronger antibody responses than two AstraZeneca shots. Both AstraZeneca and Johnson & Johnson’s vaccines use common cold viruses loaded with instructions to spark a response against the coronavirus.
But Crotty stresses that sticking with your original vaccine is reasonable, too. And he points out that vaccine effectiveness measured from large, real-world studies is stronger evidence than immune responses detected in the lab. One such study by Johnson & Johnson, announced in late September, reported that a second shot of its vaccine was 94 percent effective at keeping people from getting sick with COVID-19.
In some cases, concerns about side effects could factor into deciding whether to mix and match, says Sawyer of Rady’s. Serious side effects are rare for all three vaccines, but Pfizer and Moderna’s shots have been linked to some cases of myocarditis, inflammation of the tissue surrounding the heart, while Johnson & Johnson shots have caused some cases of severe blood clots. These symptoms, however, only show up in a few cases per million vaccinated people, and your best bet is to talk with your doctor.
“That isn’t built into the official recommendations. It is up to each individual and/or their physician to counsel them,” said Sawyer. “It’s not like CDC saying, ‘If you’ve ever had blood clots, don’t get another Johnson & Johnson (dose).’”
Am I going to have to keep getting boosters regularly?
Not necessarily, according to Sawyer and Crotty, especially if research suggesting that vaccines spark strong immune memory responses hold true. But time will tell.
“I could envision that there may be a subset of the population that needs regular doses and another group that does not,” said Sawyer, adding that those in high-risk groups may need more frequent boosters than everyone else.
CEOs for Pfizer and Moderna have both said that booster doses could become as routine as your annual flu shot. And while that’s possible, Crotty points out that it’s clearly in the self-interest of these companies to convince the public that we’ll need regular boosters.
The other major factor that will dictate how often we need boosters is the virus itself. The original strain first seen in Wuhan, China has mutated into a growing list of viral variants, from the Alpha strain, first spotted to the U.K., to Delta, originally seen in India but which now accounts for nearly all new infections in the U.S.
The virus will continue mutating. After all, that’s what viruses do. But while that’s raised fears that a new strain could arise that makes vaccines ineffective, Crotty is more optimistic.
“There’s definitely uncertainty there. The virus has had more surprises in its evolution than most of us expected,” he said. “(But) the immune escape changes that it’s had have really been a handful of changes, and those same handful keep popping up.”
Get Essential San Diego, weekday mornings
Get top headlines from the Union-Tribune in your inbox weekday mornings, including top news, local, sports, business, entertainment and opinion.
You may occasionally receive promotional content from the San Diego Union-Tribune.