Your immune system fights COVID-19 best when it fights together, La Jolla scientists report
It takes a unified front to ward off the coronavirus, and that gets harder with age
Your immune system’s best chance at fighting off the novel coronavirus is to work as a single, unified force, something that doesn’t happen as readily in older adults, according to a study published Wednesday by scientists at La Jolla Immunology.
Researchers found that those with milder cases of COVID-19 launched a multipronged counterattack against the virus, blocking infection and clearing infected cells. But the immune systems of adults 65 and older don’t do that nearly as well as younger groups.
The finding may help to explain one of the most baffling aspects of COVID-19 — why the disease puts some people on ventilators while others develop few, if any, symptoms. And authors say the lessons learned from this study could affect the kinds of immune responses researchers measure in COVID-19 vaccines trials.
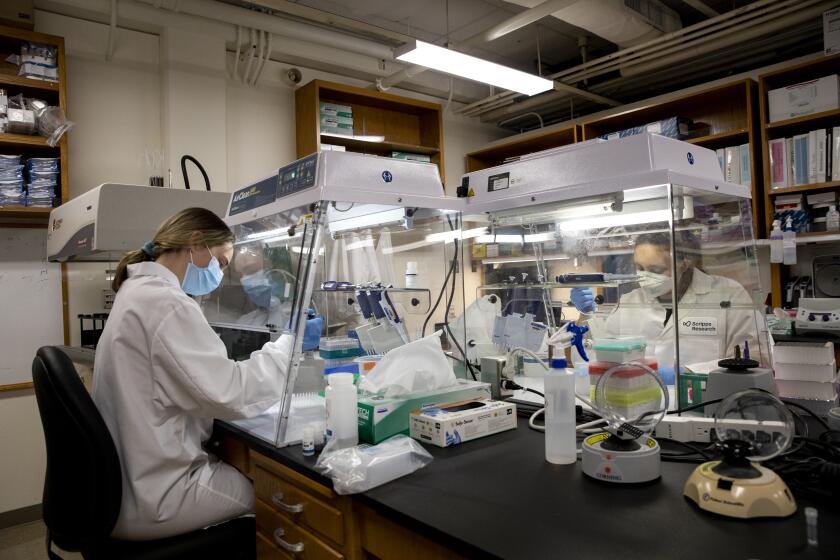
“It’s a very clean, authoritative study,” said Dennis Burton, a Scripps Research immunologist who was not involved in the work.
The scientists measured immune responses in blood samples from more than 50 San Diegans, including those who’ve recovered from COVID-19, people currently battling the disease and local residents who haven’t been exposed to the coronavirus.
From these samples, researchers looked at two key immune players: antibodies, proteins that latch onto a virus and can prevent infection, and T cells, which kill infected cells and direct the overall scale and strategy of an immune response.
A quick rundown of what antibodies can (and can’t) tell us about COVID-19
COVID-19 patients with strong antibody and T cell responses tended to have milder disease. But even a T cell response alone was helpful, though antibodies on their own were not. Most vaccine research focuses on getting the body to produce antibodies, not T cells, says Shane Crotty, the study’s senior author.
“If you have a vaccine that has a decent antibody response, but maybe can’t stop everything and you still get an infection, you really want those T cells to be present to go ahead and mop it up,” said Crotty.
Burton, who is an antibody expert, says the findings agree with what scientists have long known about how the body usually responds to viral infections.
“The first time you encounter a virus, it’s the T cells that do the job,” Burton said. “The next time, and this is the principle of vaccination, you hope the antibodies are going to kick in.”
Adults 65 and older were less likely to have dual T cell and antibody responses. Part of the issue seems to be that older adults simply have fewer T cells that can respond to new infections — a well-established aspect of how the immune system changes with age, but a disadvantage when dealing with a new virus.
The findings, Crotty says, underscore the importance of making sure any COVID-19 vaccine sparks strong T cell responses in older adults. He says that his team is eager to lend their expertise to decipher data from ongoing COVID-19 vaccine trials.
Going forward, the researchers plan to confirm their results in larger-scale studies. And they’d love to test whether the T cells most helpful in fighting off COVID-19 also recognize other coronaviruses that cause the common cold. If so, that could mean that exposure to these older cousins of the novel coronavirus protect against COVID-19.
“We almost talk about it every day,” Crotty said.
Some people who’ve never been exposed to the novel coronavirus may have protection against it, but that is far from certain
Get U-T Business in your inbox on Mondays
Get ready for your week with the week’s top business stories from San Diego and California, in your inbox Monday mornings.
You may occasionally receive promotional content from the San Diego Union-Tribune.