Abstract
Background
Extremely preterm (EPT) birth has been related to dysregulation of stress responses and behavioral/learning problems at school age. Early adverse experiences can blunt HPA axis reactivity. We hypothesized that an attenuated cortisol awakening response would be associated with developmental and behavioral problems at school age in EPT children.
Methods
This secondary analysis of a sub-cohort of the SUPPORT study included children born between 24 and 27 weeks, evaluated at 6–7 years with a neurodevelopmental battery and cortisol measures. Differences were tested between EPT and a term-born group. Relationships of cortisol awakening response to test scores were analyzed.
Results
Cortisol was measured in 110 EPT and 29 term-born 6–7 year olds. Unadjusted WISC-IV and NEPSY-II scores were significantly worse among EPT children only. Conners Parent Rating Scale behavior scores were significantly worse among EPT children. After adjusting for covariates, blunted cortisol awakening responses were found to be associated with poorer scores on memory tests and greater problems with inattention for the EPT group (p < 0.05) only.
Conclusions
Among children born EPT, we identified an association of blunted cortisol awakening response with memory and inattention problems. This may have implications related to stress reactivity and its relationship to learning problems in children born EPT.
ClinicalTrials.gov ID
Extended Follow-up at School Age for the SUPPORT Neuroimaging and Neurodevelopmental Outcomes (NEURO) Cohort: NCT00233324.
Impact
-
In children born EPT, stress reactivity may have a relationship to learning problems.
-
Cortisol awakening response should be a component for follow-up in EPT born children.
-
Components of executive function, such as memory and attention, are related to stress reactivity.
Similar content being viewed by others
Introduction
Infants born extremely preterm (EPT; 24–27 weeks gestational age) undergo numerous life-saving interventions and procedures in the neonatal intensive care unit (NICU), which can be painful or stressful. Exposures in the NICU differ greatly from those in utero and include increased exposure to sounds, lights, and other physical sensations. Infants in the NICU often undergo painful procedures increasing their cortisol levels. Many infants in the NICU also experience prolonged separation from parents who cannot be at bedside regularly, leading to stress. When stress is experienced, the hypothalamic–pituitary–adrenal (HPA) axis is activated and cortisol is released. It has been reported that preterm infants with higher observed stress, as reflected by increased Neonatal Infant Stressor Scale scores,1 have higher levels of neonatal salivary cortisol.2 However, repeated exposure to adverse experiences in the NICU can lead to disruption in the development of the HPA axis, reflected in changes in basal cortisol levels and cortisol reactivity well beyond discharge from the NICU.3,4,5,6,7,8
In other populations, early adverse experiences have been shown to lead to blunting of HPA axis reactivity,9 commonly assessed by the “cortisol awakening response,” i.e., the increase in cortisol between first awakening and 30–45 min later. In a study of children who were adopted from orphanages,9 these children had blunted cortisol awakening responses at 7–15 years of age, when the child had been adopted after the age of 16 months but not for those children adopted in infancy. This study supports the literature showing that early-life adversity can have an ongoing impact on stress response systems as measured by cortisol reactivity. We have previously reported that these 6–7 year-old children born EPT had a blunted cortisol awakening response compared to term-born children.10 We did not find an altered stress response during attending a clinic visit; however, the first cortisol sample obtained at the visit was the highest for both preterm- and term-born children, suggesting that the act of coming to the clinic visit had already been stressful.10
Chronic activation of the stress response in infancy has also been linked to changes in neurodevelopmental outcomes of term children, particularly related to executive functioning skills.11 Executive function refers to skills such as inhibition, working memory, and attention that lead to the development of goal-directed behaviors.12 Problems with executive function in young children are associated with difficulties with cognition, such as problems with sustained attention, inhibition, working memory, and behavioral dysregulation. Children born EPT are at increased risk for cognitive and behavioral difficulties in early childhood and at school age.13,14,15 Dysregulation of the HPA axis associated with exposure to a chronic and sustained elevated stress response in the NICU may partially explain this increased risk.16 In a cohort of children born very preterm, higher cortisol levels were associated with difficulty with internalizing behaviors such as emotional reactivity, attention problems, and anxious/depressive symptoms as measured by the Child Behavior Checklist at 18 months.17
Limited research is available describing the relationship between cortisol reactivity and behavior difficulties at school age in children born EPT. Neonatal pain has been found to be related to persistent altered cortisol levels in boys born preterm at 7 years.18 Greater pain exposure in preterm born children was also related to higher cortisol levels at 7 years that was associated with lower intelligence quotient scores and poorer scores on tests of visual motor integration.19 Brummelte found that increased number of painful procedures preterm children experienced at birth was associated with lower cortisol levels on study day and lower diurnal cortisol at home, specifically in boys at 7 years.20 Cortisol levels on the study day were negatively associated with attention problems and positively associated with thought problems in this same group of preterm born school-aged children. To try to address this gap in the literature, we explored whether dysregulated cortisol reactivity in children born EPT was associated with difficulties with executive functioning skills at school age. The purpose of this study was to investigate cortisol concentrations and their association with cognitive function, executive function, and behavioral challenges among school-age children born EPT in comparison to children born at term as an exploratory hypothesis-generating project. We hypothesized that children born EPT would have more difficulty on tests of cognition and executive function, in addition to higher levels of parent-reported atypical behavior when compared to children born full term. We also hypothesized that blunted awakening cortisol response at early school age would be associated with lower cognitive functioning, poorer executive function, and increased rates of reported behavior problems.
Methods
Population
The EPT children in this study had been born between 24 + 0/7 and 27 + 6/7 weeks gestation and enrolled at birth into the Surfactant Positive Airway Pressure and Pulse Oximetry Randomized Trial (SUPPORT) conducted by the Neonatal Research Network (NRN) of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. A subset of the children in the SUPPORT trial were enrolled in the Neuroimaging and Neurodevelopmental Outcomes study (ClinicalTrials.gov ID NCT00233324)21; 386 of these children had follow-up at age 6 years 4 months to 7 years 2 months. Partway through the school-age follow-up period, the National Heart, Lung and Blood Institute awarded funding to evaluate the relationship of adrenal function to perinatal factors and school-age outcomes.10 Of the preterm-born children included in the study of adrenal function, 110 had developmental and behavioral testing performed and home cortisol values obtained and are included in this report. The only significant difference between the overall group and those who returned home samples was that the education level achieved was higher in the mothers of the preterm-born group who returned home samples.10
Participants were evaluated at 15 NRN centers after parental consent was obtained. The study was approved by the Institutional Review Board of each study site. Perinatal data were obtained from the original study database. A comparison group of children, born healthy at term, were recruited from 5 NRN sites (n = 40). Of the 40 term-born children, 29 had home cortisol values and were included in this study. Children born full term were eligible based on the following criteria: (1) singleton birth with 5th to 95th percentile birth weight and 37–41 weeks gestation; (2) 6 years 4 months to 7 years old; (3) 5th to 95th percentile for height and weight; (4) never hospitalized >2 days; (5) without known medical problems; (6) never identified as eligible for special education, speech, or physical therapy; (7) without a sibling with autism or intellectual disability; and, (8) living with their birth parent(s).
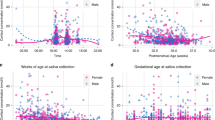
Cortisol collection
As part of a study of salivary cortisol in this population, kits were sent home after the study visit for the parents to collect specimens to measure cortisol upon awakening and 30 min later. Parents were given an instruction brochure with pictures illustrating the procedures and asked to enter the exact times of specimen collection. The time of collection was documented by parental report. 95% of specimens had times recorded, with the post-awakening specimen collected at 30 [23–46] min (median) [5–95% confidence interval] after awakening.
Saliva was collected by passive drool. If the child ate or drank anything <30 min before sampling, the child rinsed their mouth thoroughly before sampling. Samples were frozen at −20 °C, then sent to the Institute for Interdisciplinary Salivary Bioscience Research, where they remained at −80 °C until assayed in duplicate using commercially available immunoassays designed for use with saliva (Salimetrics LLC, Carlsbad, CA). The test volume was 25 μl, with lower limits of detection 0.007 mcg/dl. The intra-assay CV% was 7.55% and the inter-assay CV% as based on the validation of the assay was 6.00%.
Cortisol awakening responses were calculated by the area under the curve (AUC) between cortisol measures upon first awakening and 30 min later, with a blunted cortisol response defined as a lower AUC.9
Cognitive test measures
The Wechsler Intelligence Scale for Children—fourth edition (WISC-IV)22 was administered to each child, and composite scores in the areas of verbal comprehension, perceptual reasoning, working memory, and processing speed were obtained. All scores were standardized based on the chronological age of the child, with a mean of 100 and standard deviation of 15.
Selected subscales of the NEuroPSYchological Assessment (NEPSY-II)23 were administered. The test of auditory attention span was divided into a score of correct answers and a total score that took time into account. The test of memory for names was used, both for short- and long-term recall. All scores were standardized and converted to a t-score with a mean of 50 and standard deviation of 10 for analyses.
The Conners Parent Rating Scale24 measures parent-reported behaviors related to inattention, hyperactivity/impulsivity, learning problems, executive functioning, defiance/aggression, and peer relations. The questionnaire was computer scored and standard scores were calculated based on the child’s chronological age. The scores were converted to t-scores with a mean of 50 and standard deviation of 10. Scores >60 (84th percentile) were considered moderately elevated and scores >70 (98th percentile) were considered significantly elevated.
Statistical analysis
Differences in maternal and child characteristics between children born EPT and term were tested by chi-square and Wilcoxon tests. The relationship between the cortisol awakening response and each cognitive and behavioral test measure was analyzed using generalized linear mixed models adjusting for center, birth weight Z scores, sex, maternal education, and the time of day the cortisol level was obtained. Reduced models only adjusted for time of day, whereas full models adjusted for all covariates listed.
Results
Table 1 describes pertinent maternal and child characteristics at birth and follow-up. The preterm born children had significantly lower birth weights and gestational ages compared to the term children. In addition, maternal education was significantly higher in mothers of term-born children. Therefore, maternal education level was adjusted for in all analyses. We previously published data from this cohort showing that the preterm-born children had significantly lower morning values with a blunted awakening response (geometric mean 22% lower at awakening and 10% lower after 30 min).10
The term-born children had higher scores on all scales of the WISC-IV and NEPSY-II, indicating higher functioning in the areas assessed. The term-born group had significantly lower scores on the Conners scale, which indicated fewer behavioral problems in the areas assessed. (Table 2)
Regression models showing the association of cortisol awakening response with developmental test scores are shown in Table 3. There was no significant relationship for the term-born group on any of the measures. However, among the EPT group, there was a significant positive association between WISC-IV verbal comprehension scores and morning cortisol AUC in the reduced model, which adjusted for time of awakening (β (SE: 0.70 (0.35), p = 0.05)). Significance was lost after further adjusting for center, sex, birth weight, and maternal education in the full model. On the NEPSY Memory for Names scale, both immediate recall (β (SE: 3.84 (1.88), p = 0.04)) and delayed recall (β (SE: 4.81 (1.95), p = 0.02)) were significantly positively associated with morning cortisol AUC in both models for the EPT group even after adjusting for all covariates. On the Conners scale, there was a significant association in the reduced model for the EPT group (such that lower/blunted awakening response was associated with increased scores) for inattention, learning problems, and defiance/aggression. Significance was maintained in the full model for the inattention scale (β (SE: −0.86 (0.37), p = 0.02)).
Discussion
In this study, we found that children born EPT, compared to those born full term, had increased rates of cognitive, executive function, and behavior problems even after adjusting for maternal education. These findings are consistent with the literature showing that prematurity is associated with lower scores on tests of cognition and executive functioning at school age.25,26 EPT children have also been found to have increased problems with behavior, including externalizing (aggression, hyperactivity) and internalizing (anxiety, withdrawal) behaviors from preschool through school age.27,28 These problems can be associated with learning difficulties and executive function abnormalities related to attention, impulsivity, and self-regulation.29
The association of learning and behavioral problems with cortisol awakening response has been infrequently studied. We previously reported that this cohort of children born EPT showed a blunted cortisol awakening response, compared to those born at term gestation. We now report that there was a significant association of morning cortisol awakening response with verbal comprehension and verbal memory in the EPT group. After adjusting for center, birth weight, sex, and socio-economic factors, the memory scores maintained a significant association with cortisol. In areas of behavior, only the EPT group had a significant association between cortisol awakening response and behavioral scores in areas of inattention, learning problems, and aggression. Similarly, after adjusting for the above factors, a significant association with cortisol was maintained only for inattention.
Children born preterm, having experienced noxious exposures in the NICU, may display disruption in HPA axis function throughout childhood. Indicators of this dysregulated stress response in the HPA axis include blunting of morning cortisol levels10 and reduced cortisol reactivity in response to stress.9 Children with adverse early-life experiences display a blunted cortisol awakening response and changes in cortisol reactivity in response to stressors throughout the day.30
A systematic review found that, among toddlers and early school age children born EPT, those with greater exposures to painful procedures during the neonatal period displayed poorer neurodevelopmental outcomes and disruptions in their cortisol activation compared to those with lower numbers of painful procedures.8 In another study of school age children with a history of preterm birth, children born very preterm (under 32 weeks), did not display overall differences in diurnal patterns or in cortisol reactions to stress in comparison to children born full term; however, further analyses revealed that those born preterm who had experienced more pain-related stress in the neonatal period displayed lower cortisol levels throughout the day than their peers born full term or preterm without pain-related stress in the NICU.20 Furthermore, in the same study, children born preterm who displayed attention problems had lower levels of cortisol reactivity in response to stress. Our study also found that the children born EPT had an association of lower awakening cortisol AUC with increased inattention problems at 6–7 years, possibly related to differences in cortisol reactivity associated with stress experienced in the neonatal period.
Strengths of this study included a multi-center trial with a large cohort of EPT children with assessments completed by psychologists who underwent comprehensive training for inter-rater reliability. Limitations included a higher level of maternal education in the term control group, which was included in the regression models. A single parent questionnaire was used to measure the child’s behavior problems, whereas multimodal assessment, including teacher ratings, may have provided a more comprehensive understanding of a child’s behavioral functioning. Parents’ interpretations of the questions and their own psychological functioning could have influenced their responses; however, the Conners scale is widely used both in research and in the clinical setting and is considered a robust measure of behavior. Finally, this study started part way through the NEURO school-age study period; however, population characteristics and neonatal morbidities were similar between this group and the overall NEURO population with the exception that the adrenal study group had a lower incidence of intraventricular hemorrhage/periventricular leukomalacia (7 vs 9%).
In conclusion, our findings of an association between the cortisol awakening response and developmental outcomes in children born preterm, specifically in areas of memory and inattention, provides important information related to potential consequences of early stress. Further investigation of both parental and neonatal stress, as well as strategies to mitigate those stressors, may provide additional insight into the mechanisms contributing to this association. Enhanced support of children born preterm and their families, especially those from homes with limited resources, may be beneficial to the preterm child’s learning and behavior outcomes.
Data availability
Data reported in this paper may be requested through a data use agreement. Further details are available at https://neonatal.rti.org/index.cfm?fuseaction=DataRequest.Home.
References
Newnham, C. A., Inder, T. E. & Milgrom, J. Measuring preterm cumulative stressors within the NICU: The Neonatal Infant Stressor Scale. Early Hum. Dev. 85, 549–555 (2009).
Pourkaviani, S. et al. Clinical validation of the Neonatal Infant Stressor Scale with preterm infant salivary cortisol. Pediatr. Res. 87, 1237–1243 (2020).
Provenzi, L. et al. Pain-related stress in the Neonatal Intensive Care Unit and salivary cortisol reactivity to socio-emotional stress in 3-month-old very preterm infants. Psychoneuroendocrinology 72, 161–165 (2016).
McLean, M. A. et al. Sensory processing and cortisol at age 4 years: procedural pain-related stress in children born very preterm. Dev. Psychobiol. 63, 915–930 (2021).
Brummelte, S. et al. Cortisol levels in relation to maternal interaction and child internalizing behavior in preterm and full‐term children at 18 months corrected age. Dev. Psychobiol. 53, 184–195 (2011).
Kaseva, N. et al. Adrenalin, noradrenalin and heart rate responses to psychosocial stress in young adults born preterm at very low birthweight. Clin. Endocrinol. 81, 231–237 (2014).
Grunau, R. E. Neonatal pain in very preterm infants: long-term effects on brain, neurodevelopment and pain reactivity. Rambam Maimonides Med. J. 4, 1–13 (2013).
Valeri, B. O., Holsti, L. & Linhares, M. B. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin. J. Pain. 31, 355–362 (2015).
Leneman, K. B., Donzella, B., Desjardins, C. D., Miller, B. S. & Gunnar, M. R. The slope of cortisol from awakening to 30 min post-wake in post-institutionalized children and early adolescents. Psychoneuroendocrinology 96, 93–99 (2018).
Watterberg, K. L. et al. Adrenal function links to early postnatal growth and blood pressure at age six in children born extremely preterm. Pediatr. Res. 86, 339–347 (2019).
Wagner, S. L. et al. Higher cortisol is associated with poorer executive functioning in preschool children: The role of parenting stress, parent coping and quality of daycare. Child Neuropsychol. 22, 853–869 (2016).
BussKara, A. T. & Lowery N. in Encyclopedia of Infant and Early Childhood Development (Second Edition) (Haith, M. M. & Benson, J. B.) 183–193 (Academic, 2020).
Cassiano, R. G. M., Gaspardo, C. M. & Linhares, M. B. M. Temperament moderated by neonatal factors predicted behavioral problems in childhood: a prospective longitudinal study. Early Hum. Dev. 135, 37–43 (2019).
Hutchinson, E. A., De Luca, C. R., Doyle, L. W., Roberts, G. & Anderson, P. J. School-age outcomes of extremely preterm or extremely low birth weight children. Pediatrics 131, e1053–e1061 (2013).
Rogers, E. E. & Hintz, S. R. Early neurodevelopmental outcomes of extremely preterm infants. Semin. Perinatol. 40, 497–509 (2016).
Grunau, R. E. et al. Altered basal cortisol levels at 3, 6, 8 and 18 months in infants born at extremely low gestational age. J. Pediatr. 150, 151–156 (2007).
Brummelte, S. et al. Cortisol levels in relation to maternal interaction and child internalizing behavior in preterm and full-term children at 18 months corrected age. Dev. Psychobiol. 53, 184–195 (2011).
Grunau, R. E. et al. Neonatal pain-related stress and NFKBIA genotype are associated with altered cortisol levels in preterm boys at school age. PLoS ONE 8, e73926 (2013).
Chau, C. M. Y. et al. The Val66Met brain-derived neurotrophic factor gene variant interacts with early pain exposure to predict cortisol dysregulation in 7-year-old children born very preterm: implications for cognition. Neuroscience 342, 188–199 (2017).
Brummelte, S. et al. Cortisol levels in former preterm children at school age are predicted by neonatal procedural pain-related stress. Psychoneuroendocrinology 51, 151–163 (2015).
Hintz, S. R. et al. Preterm neuroimaging and school-age cognitive outcomes. Pediatrics 142, e20174058 (2018).
Wechsler, D. Wechsler Intelligence Scale for Children: Fourth Edition (WISC-IV) (PsychCorp 2003).
Korkman, M., Kirk, U. & Kemp, S. NEPSY-II: Clinical and Interpretation Manual (Pearson Corp, 2007).
Conners, C. K. Conners’ Rating Scales–Revised: Technical Manual (Multi-Health Systems 1997).
Odd, D., Evans, D. & Emond, A. M. Prediction of school outcome after preterm birth: a cohort study. Arch. Dis. Child. 104, 348–353 (2019).
Linsell, L. et al. Trajectories of behavior, attention, social and emotional problems from childhood to early adulthood following extremely preterm birth: a prospective cohort study. Eur. Child Adolesc. Psychiatry 28, 531–542 (2019).
Schappin, R., Wijnroks, L., Uniken Venema, M. & Jongmans, M. Exploring predictors of change in behavioral problems over a 1- year period in preterm born preschoolers. Infant Behav. Dev. 50, 98–106 (2018).
Dotinga, B. M. et al. Longitudinal growth and emotional and behavioral problems at age 7 in moderate and late preterms. PLoS ONE 14, e0211427 (2019).
Brumbaugh, J. E., Hodel, A. S. & Thomas, K. M. The impact of late preterm birth on executive function at preschool age. Am. J. Perinatol. 31, 305–314 (2014).
Raffington, L. et al. Blunted cortisol stress reactivity in low–income children relates to lower memory function. Psychoneuroendocrinology 90, 110–121 (2018).
Acknowledgements
Participating NRN sites collected data and transmitted it to RTI International, the data coordinating center (DCC) for the network, which stored, managed, and analyzed the data for this study. On behalf of the NRN, RTI International had full access to all of the data in the study, and with the NRN Center Principal Investigators, takes responsibility for the integrity of the data and accuracy of the data analysis. We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study.
Funding
The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Heart, Lung, and Blood Institute (NHLBI) provided grant support for the Neonatal Research Network’s Extended Follow-up at School Age for the SUPPORT Neuroimaging and Neurodevelopmental Outcomes (NEURO) Cohort through cooperative agreements. While NICHD staff had input into the study design, conduct, analysis, and manuscript drafting, the comments and views of the authors do not necessarily represent the views of NICHD, the National Institutes of Health, the Department of Health and Human Services, or the U.S. Government.
Author information
Authors and Affiliations
Consortia
Contributions
J.L. and K.L.W.: conception and design, acquisition, analysis and interpretation of data, drafting the article, and final approval of the version to be published. J.F.F.: acquisition of data, critical revision of the article for important intellectual content, and final approval of the version to be published. A.D.: conception and design, drafting the article and final approval of the version to be published. B.D. and A.G.D.: analysis and interpretation of the data, revising it critically for important intellectual content, and final approval of the version to be published. C.M.B.: analysis and interpretation of the data, revising it critically for important intellectual content, final approval of the version to be published. K.E.G.: substantial contributions to conception, design, acquisition of data, drafting the article revising it critically for important intellectual content, and final approval of the version to be published. B.R.V.: acquisition and interpretation of data, critical revision of the article for important intellectual content, and final approval of the version to be published. S.R.H.: conception and acquisition of the data, revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
A.G.D. is founder and chief scientific and strategy advisor at Salimetrics LLC and Salivabio LLC. The nature of those relationships is managed by the policies of the committees on conflict of interest at the Johns Hopkins University School of Medicine and the University of California at Irvine.
Ethics approval and consent to participate
Patients were consented at each institution per each institution’s IRB requirements.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lowe, J., Fuller, J.F., Dempsey, A.G. et al. Cortisol awakening response and developmental outcomes at 6–7 years in children born extremely preterm. Pediatr Res 93, 689–695 (2023). https://doi.org/10.1038/s41390-022-02113-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02113-9