Curriculum-at-a-Glance
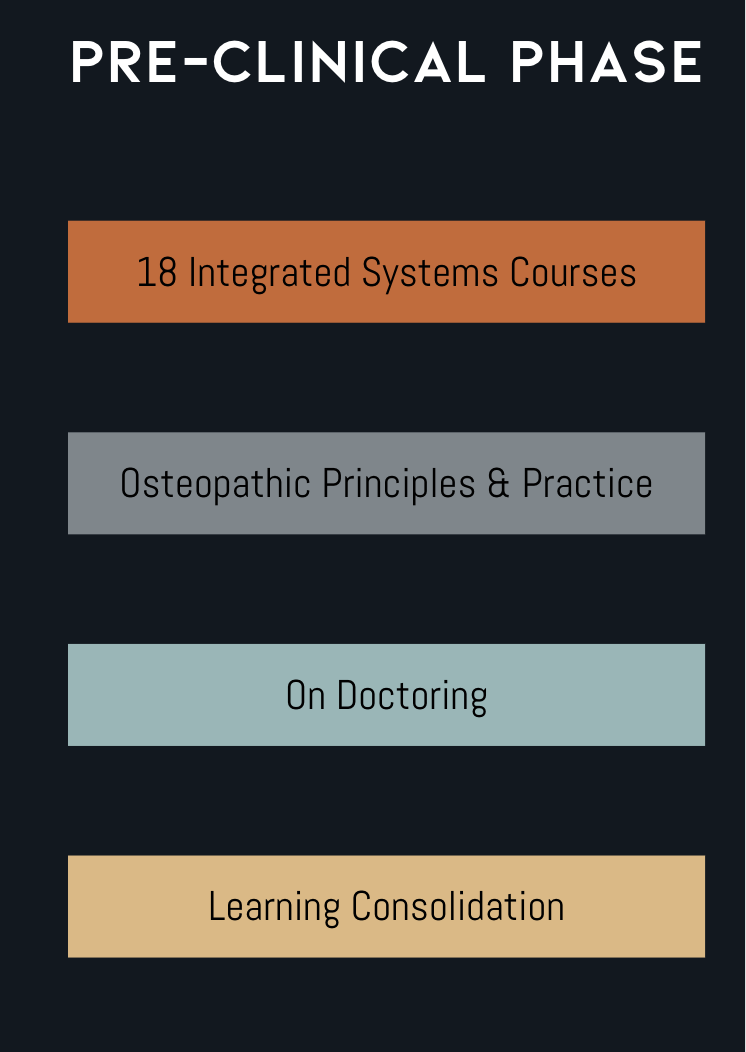
Pre-Clinical Phase
During the Pre-Clinical Phase, students will cover the following topics and courses during their first two years:
Clinical Phase
The Clinical Phase (years 3 and 4) focuses on integrating and expanding the knowledge of the medical student through patient experiences under the supervision of clinical faculty. There are asynchronous and self-directed learning experiences integrated into the required third-year rotations.
Curriculum Philosophy & Strategies
OCOM will award grades on a Pass/Fail grading system. We advance our mission through a carefully planned “lecture-less” systems-based curriculum that takes an evidence-based approach to educating osteopathic medical students and incorporates the following:
Active Retrieval/Frequent Assessment;
Spaced Practice, Interleaved Learning and Practice, and Spiral-Based Education,
Variation of Learning Strategies;
Effortful/Active Learning;
Integration of Elaboration, Generation, Reflection, and Learning Devices; and
Use of Multiple, Objective Measures to Provide Timely Feedback on Learning.
To accomplish these principles, we implement the following strategies:
A systems-based approach integrating clinically applicable biomedical science concepts into the clinical application of medical knowledge;
Use of a combination of:
Case-based learning;
Flipped classroom education;
Team-based learning;
Formative assessments;
Active assessment practices (question banks);
Simulation-based learning;
Weekly quizzes/assessments;
Ongoing summative assessment/learning consolidation and
Objective structured clinical examinations (OSCEs) throughout the curriculum.
Patient-Centered Education
Patient-centered education is used throughout the OCOM educational model, where all aspects of medical education integrate the biomedical sciences and are applied to clinical scenarios to garner higher learning outcomes using critical thinking led by experienced clinicians. Vertical and horizontal integration facilitates linkage between course and clinical work across the four years of the curriculum. We believe strongly that the clinical application of basic and biomedical sciences offers a superior approach to traditional learning approaches, such as straight recall. By having in place admission pre-requisites, we do not need to recreate undergraduate courses in our curriculum; rather, we create just-in-time learning opportunities to ensure that all students are prepared for clinical discussions.
Vertical integration refers to interweaving clinical skills and knowledge into the basic science years and, in turn, reinforcing basic science concepts as they apply during the clinical years. Horizontal integration refers to identifying concepts or skills, particularly those that are clinically relevant, that cut across the basic sciences, and then using these as an integrated focus for learning sessions, clinical scenarios, and course materials.
Curriculum Development
OCOM faculty members develop the curriculum with input from the larger college Curriculum Committee and the Department Chairs and Course Directors. Integration is ensured by Course Directors and Course Teams of subject matter experts (individualized for each course) overseeing the appropriateness of the content. A Course Leadership Liaison assists in the organization and operationalization of the curriculum and supports the Associate Dean of Pre-Clinical Education in ensuring that faculty have the tools they need to succeed in delivering their content to our students.
Curricular Documents
Frequently Asked Questions
-
The curriculum is developed in a way that prepares students for both the challenges of residency as well as the realities of needing to pass medical licensing examinations. The curriculum is based off of the AOA's Seven Core Osteopathic Competencies and is a systems-based curriculum with integrated biomedical science themes weaved throughout.
-
No. Like many modern medical school curricula, OCOM will not have mandatory in-person lectures. Watching a lecture is a form of passive learning. Evidence exists which tells us that virtual attendance at these types of sessions (content delivery sessions) actually portends better learning outcomes than in-person attendance since the student can control the speed of the lecture, go back to review something that was missed or challenging, etc. Therefore, OCOM’s curriculum will consist of self-directed learning sessions which are pre-recorded “lecture-like” sessions assigned to watch as part of the self-directed learning experience. Students will be able to watch these on their own time. Then, while in on campus sessions, students will be challenged by faculty to apply what they have learned on their own.
-
Basic science is critical to the foundational understanding of medicine for any student; in that vein, it will largely be taught in an integrated manner within the body system courses, with some exceptions, such as anatomy which will be introduced up-front in the Foundations course, and then brought through into the various courses longitudinally in a just-in-time manner. Basic sciences will be stressed in the Foundations course, and at the start of each system.
-
The curriculum at OCOM has been carefully crafted to form a firm, stable scaffolding of knowledge upon which students can build their own individual knowledge outward through vertical and horizontal curricular integration in the first two years in a lecture-less curriculum. The curriculum employs a spiral method of assessment and delivery in which a concept may be taught in the spring of year 1, but may come up on an assessment or CBL case in spring of year 2, necessitating students to continually review past information to strengthen their scaffolding of knowledge to the point where they are able to seamlessly transition from on-campus to hospital-based education, and also excel on the COMLEX-USA examination series.
-
The educational style we have built our curriculum around is called andragogy, which is an adult learning principle that supports self-directed learning, inquiry, and discovery, while providing pedagogical guideposts and opportunities to apply knowledge longitudinally. For instance, CBL sessions will be facilitated by faculty who are experts in their field, and these cases will challenge our students to apply the knowledge gained from self-directed learning to clinical/patient-based scenarios in order to prepare students for the realities of clinical medicine and support their development into a strong Year 3 clinical student.
-
Assessment at OCOM will be done weekly in the form of quizzes, and episodically in the form of examinations, with examinations in the Consolidation courses being spiral and cumulative over all content learned throughout the previous courses at OCOM. These exams will challenge students to integrate knowledge into clinical contexts, mirroring Year 3 rotations, and questions will be designed similarly to those found on the COMLEX-USA. In the systems, exams will occur at the end of each system, and for systems of 4-week duration or greater, at the half-way mark in the course. On Doctoring and OPP course examination sequences will vary based upon the material being tested.
-
The best way to visualize the Foundations Course is a clinically-oriented approach to basic science knowledge presented in a clinical context to prepare students for the systems based education to come. In that vein, it is dissimilar to most content covered in an undergraduate curriculum.