Column One: How does COVID-19 change the brain? This scientist is finding out

In a room as cold as a refrigerator, Dr. Maura Boldrini bends over a plastic box filled with pale slices of human brain, each piece nestled in its own tiny, fluid-filled compartment.
She gestures with purple-gloved fingers: Here are the folds of the cortex, where higher cognition takes place. There is the putamen, which helps our limbs move. Here is the emotion-processing amygdala, with its telltale bumps.
Each piece in this box came from a single brain — one whose owner died of COVID-19.
There are dozens more containers just like it stacked in freezers in Boldrini’s lab at the New York State Psychiatric Institute.
“Each of these boxes is one person,” she says in a lilting Italian accent. Each will play a crucial role in helping to unravel COVID-19’s effects on the brain.
The disease may be best known for its ability to rob people of their breath, but as the pandemic spread, patients began reporting a disconcerting array of cognitive and psychiatric issues — memory lapses, fatigue and a mental fuzziness that became known as brain fog. There were also more acute problems, including paranoia, hallucinations, thoughts of suicide and psychosis.
This strange constellation of symptoms has led researchers to suspect that the disease is mounting a direct attack on the brain. Researchers want to figure out how — and what the assault’s long-term effects may be.
Boldrini, a neuroscientist at Columbia University, studies the biology of suicide and the physiological markers of resilience in brain tissue. She is also a practicing psychiatrist.
That combination makes her uniquely suited to investigate the underpinnings of "long COVID." She has gathered more than 40 brains from COVID-19 victims to guide her in her quest.
What Boldrini and her colleagues learn could have implications far beyond COVID-19, shedding light on mental illness, the origins of dementia and the myriad ways viral infections affect the brain.
To unlock the disease’s secrets, they’ll have to carefully take each brain apart, count its cells, track its gene expression and document its proteins.
“We have a lot of work to do,” Boldrini says.
::
New York City was one of the coronavirus' early targets, and it didn't take long for Boldrini to notice surprising issues among COVID-19 patients, including serious mood and psychiatric symptoms.
“Very strange symptoms,” she recalls — made even stranger because they were cropping up in people with no personal or family history of such problems. Adding to the mystery was the appearance of these conditions relatively late in a patient’s life rather than in adolescence and early adulthood.
I feel like this dread that I'm feeling is something organic in my brain, one patient told her. Psychologically, I'm not anxious about anything.
“It's a very different kind of symptomatology compared to people that have normal anxiety,” Boldrini says.

Then there were the rarer, but more disturbing, cases of suicidal ideation.
Boldrini has not encountered a COVID-19 patient who died of suicide. But one case did hit her university close to home: Dr. Lorna Breen, an emergency department physician at Columbia who worked on the front lines before becoming ill herself during the pandemic's brutal first wave.
Breen was a talented and dedicated doctor who took up snowboarding and salsa dancing in her spare time. Shortly after returning to work, her mental health deteriorated and she died by suicide within weeks.
“She had COVID, and I believe that it altered her brain,” her sister Jennifer Feist said on NBC's "Today" last year.
If so, how?
Researchers have found signs that the virus can establish a foothold of sorts on the periphery of the brain, where the protective blood-brain barrier opens up to allow key molecules to slip through. One of those places is the olfactory bulb, which can be reached through the nose — a fact that could explain why so many COVID-19 patients lose their sense of smell.
Yet scientists have so far found little evidence that the virus penetrates any deeper than that. Instead, they’ve seen the type of damage caused by strokes, as well as the blood clots that may have precipitated them.
That’s part of why Boldrini and many others suspect that inflammation — the immune system’s all-hands-on-deck response to an invader — may play an essential role in the brain damage experienced by COVID-19 patients.
Inflammation can trigger blood clots, and once a clot forms, inflammation increases around it. It’s similar to what’s seen in people who experience traumatic brain injury, including football players, military veterans and victims of car accidents.
“People that have this kind of trauma in the brain have presented with sudden changes in behavior and personality and suicide and other brain symptoms,” Boldrini says. It’s eerily similar to what many COVID-19 patients face — and she doesn’t think that’s a coincidence.
::
To gain a deeper understanding of what’s happening on a cellular and molecular level, scientists need to study the brains of people who died of COVID-19. But Boldrini prefers not to work with brains collected by others — she has to know everything about how the tissue was collected and preserved so she can understand the results of her experiments.
"Depending how you freeze, store and fix the brain, you can get very different results,” she says.
At Columbia, she and her colleagues examine tissue from autopsies, so they have complete control over how the precious tissue is handled.
Boldrini wants to know which genes were being expressed; to track molecular markers of inflammation; to see how microglia — the brain's immune cells — were behaving; and to document the state of the neurons and their connections with one another.

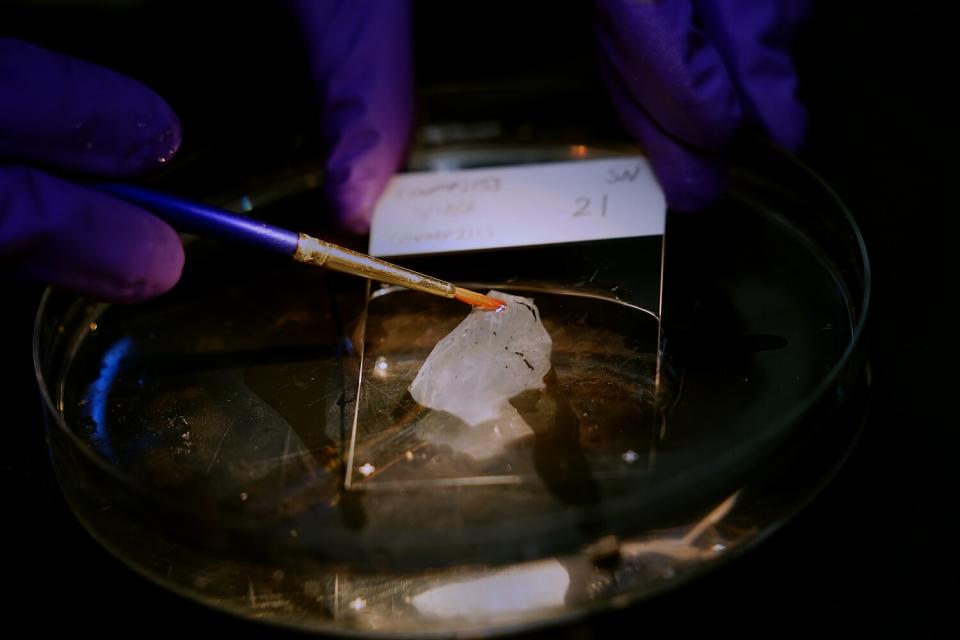
Mapping the multifaceted effects of one disease is an ambitious endeavor, and it requires painstaking work. One of the students working in the lab starts by taking a scallop-edged sample of the amygdala and mounting it on a bed of dry ice. Drop by drop, she coats the tissue in sugar water, which eventually freezes and holds the sample in place.
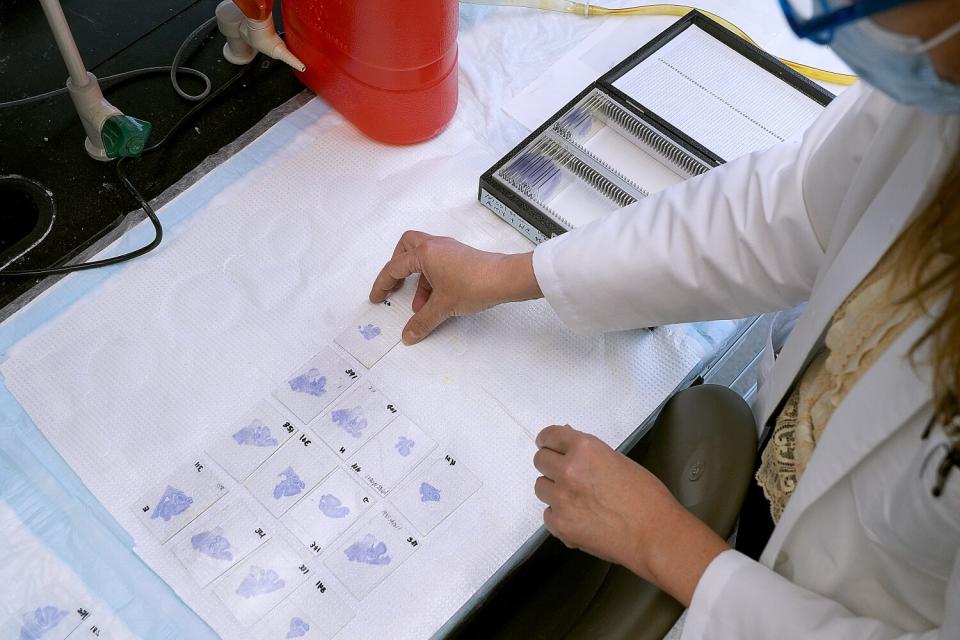
Next, she slices off pieces that are a mere 50 microns thick — just wide enough to contain a single layer of brain cells. Each fragile cut is then submerged in water and centered on a glass slide with fine-tipped paintbrushes.
The slides are stained with dyes that allow the researchers to see different types of cells in the tissue. Those cells are counted under a microscope, partly by human eye and partly with the help of a computer algorithm.
Boldrini looks over the student’s shoulder at one of the slides magnified on a computer screen. This slice of brain tissue resembles a galactic crush of stars stretched across a darkened sky: The scattered blue stars are glia, the brain’s protective cells. The green ones are neurons, densely packed together. The red stars are young, immature neurons.
“It’s beautiful,” Boldrini says. “Anatomy is very beautiful.”

The red stars are the rarest of the three, and they're even more sparse in many patients who had COVID-19 — about 10 times less abundant. That’s a problem because these young neurons are necessary for learning and memory, for coping with stress, and for integrating memories with emotions.
Boldrini suspects these immature cells are done in by stress hormones and inflammation.
“This would explain the brain fog,” she says.
A few days earlier, the researchers went through the same steps with the hippocampus, a tiny, delicate brain structure involved in mood and memory.
Other scientists have found that COVID-19 damages the hippocampus. That could help explain why some patients have lingering issues with depression and anxiety.
If this damage is caused by inflammation, it probably wreaks havoc in several ways. Scientists suspect it disrupts the flow of serotonin, a hormone that’s implicated in depression, and prompts the body to make kynurenine instead, even though it's toxic to neurons.
Inflammation also triggers coagulation, creating clots that can block blood flow to cells and kill them. And it activates the microglia, which may attempt to remove more neurons than they normally would.
Boldrini’s work will help scientists disentangle the factors driving that damage.
“She’s an expert at that,” says Dr. James Goldman, a neuropathologist at Columbia University. “We’re looking forward to seeing what she comes up with.”
::
In a nearby room, research assistant Cheick Sissoko checks to see whether the DNA fragments obtained from the tissue are too big or too small for proper analysis. If they're the right size, Sissoko will use them to better understand the gene expression in these brain cells — particularly in the young neurons that seem to be taking a hit in COVID-19 patients.
"Ideally, we can look at every single gene expressed by a single cell," he says.

On other days, Sissoko focuses on RNA, the molecule that helps turn DNA’s instructions into actual proteins. The RNA contained in brain tissue may provide clues about the alarms that were set off in the body in response to the coronavirus, and how the body reacted to a perceived threat.
Sissoko uses a sophisticated new technique to sequence the RNA on a slide-by-slide basis. That allows him to see how RNA expression changes in different parts of the brain.
Ultimately, the researchers aim to combine the data on RNA, the microglia, the new and mature neurons, and the connections they make to create a portrait of a brain ravaged by COVID-19.
By comparing the brains of COVID-19 patients with and without neurological symptoms, Boldrini hopes to shed light on the role of inflammation in a wide swath of neurodegenerative diseases, including depression and dementia.
“This pandemic is almost like a natural experiment where you have a lot of inflammation like in a very unusual way,” she says. “We hope that this is going to clarify some mechanisms of brain damage independently of COVID itself.”
That, in turn, may help people understand that mental health is a crucial part of physical health.
“I think this could be very useful to fight the stigma against psychiatric illness,” Boldrini says. “The brain is an organ, like any other one.”
Dr. Christian Hicks Puig, a psychiatrist at Columbia Medical Center who works at the long COVID clinic, agreed. Many mental health issues are rooted in biological processes. “It's all extremely interconnected,” he says.
As researchers such as Boldrini map COVID-19's assault on the brain, they may help doctors more deeply understand the relationships among mental health, cognitive health and disease. They may also gain insight into the long-term needs of COVID-19 survivors.
That progress would not be possible without the contributions of those who didn't make it, Goldman says.
"We are very, very grateful to families who have allowed us to do these autopsies," he says.
Boldrini agrees, adding that she and others feel immense pressure to handle these organs with care.
“These are people,” she says. What they reveal about COVID-19 is crucial. What they represent is irreplaceable.
This story originally appeared in Los Angeles Times.

