Abstract
Background
The minimal literature on the relation between chronic pain and both eudaimonic (EWB) and hedonic well-being (HWB) examines the relation cross-sectionally, and most studies have examined chronic pain’s effect only on psychopathology.
Methods
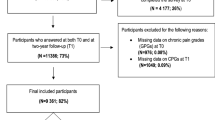
Using a sample of 473 midlife and older adults with chronic pain, this study examined both the cross-sectional and longitudinal relations between chronic pain and EWB and HWB in addition to psychological distress.
Results
Multiple-group longitudinal structural equation modeling revealed that chronic pain was related significantly and negatively to EWB and HWB, and significantly and positively to distress among both men and women. When examined longitudinally, chronic pain at time 1 was associated significantly only with decreased EWB at time 2, suggesting chronic pain’s risk to psychological functioning, especially because of its long-term effects on future EWB.
Conclusions
Our study provides a comprehensive picture of the way chronic pain is associated both with EWB and HWB, in addition to psychological distress. Further, chronic pain may have a lasting influence on EWB, while it may have little predictive value for future HWB and psychological distress. Our study supports well-being’s relevance to chronic pain research and has the potential to guide prevention strategies and treatment for chronic pain using a positive psychological framework.


Similar content being viewed by others
References
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156:1003–7.
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–24.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133:581–624.
Gatchel RJ. Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am Psychol. 2004;59:795–805.
Huber A, Suman AL, Biasi G, Carli G. Predictors of psychological distress and well-being in women with chronic musculoskeletal pain: two sides of the same coin? J Psychosom Res. 2008;64:169–75.
McBeth J, Macfarlane GJ, Silman AJ. Does chronic pain predict future psychological distress? Pain. 2002;96:239–45.
Karapetyan AA, Manvelyan HM. Chronic pain and depression. In: Breznoscakova D, editor. Depression. London, United Kingdom: InTech; 2017. p. 55–68.
Meeks TW, Dunn LB, Kim DS, Golshan S, Sewell DD, Atkinson JH, et al. Chronic pain and depression among geriatric psychiatry inpatients. Int J Geriatr Psychiatry. 2008;23:637–42.
Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9:883–91.
Carleton RN, Afifi TO, Taillieu T, Turner S, El-Gabalawy R, Sareen J, et al. Anxiety-related psychopathology and chronic pain comorbidity among public safety personnel. J Anxiety Disord. 2018;55:48–55.
Diener E. Hedonic well-being. Psychol Bull. 1984;95:542–75.
Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52:141–66.
Diener E, Suh EM, Lucas RE, Smith HL. Hedonic well-being: three decades of progress. Psychol Bull. 1999;125:276–302.
Carruthers CP, Hood CD. The power of the positive: leisure and well-being. Ther Recreat J. 2004;38:225–45.
Compton WC, Smith ML, Cornish KA, Qualls DL. Factor structure of mental health measures. J Pers Soc Psychol. 1996;71:406–13.
Baker TA, Buchanan NT, Small BJ, Hines RD, Whitfield KE. Identifying the relationship between chronic pain, depression, and life satisfaction in older African Americans. Res Aging. 2011;33:426–43.
Dezutter J, Robertson LA, Luyckx K, Hutsebaut D. Life satisfaction in chronic pain patients: the stress-buffering role of the centrality of religion. J Sci Study Relig. 2010;49:507–16.
Dezutter J, Luyckx K, Wachholtz A. Meaning in life in chronic pain patients over time: associations with pain experience and psychological well-being. J Behav Med. 2015;38:384–96.
Mangelli L, Gribbin N, Büchi S, Allard S, Sensky T. Psychological well-being in rheumatoid arthritis: relationship to ‘disease’ variables and affective disturbance. Psychother Psychosom. 2002;71:112–6.
Huppert FA. Psychological well-being: evidence regarding its causes and consequences. App Psychol Health Well Being. 2009;1:137–64.
Greenspoon PJ, Saklofske DH. Toward an integration of hedonic well-being and psychopathology. Soc Indic Res. 2001;54:81–108.
Nes RB, Czajkowski N, Roysamb E, Reichborn-Kjennerud T, Tambs K. Well-being and ill-being: shared environments, shared genes? J Posit Psychol. 2008;3:253–65.
Ryff CD, Love GD, Urry HL, Muller D, Rosenkranz MA, Friedman EM, et al. Psychological well-being and ill-being: do they have distinct or mirrored biological correlates? Psychother Psychosom. 2006;75:85–95.
McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. 2004;111:77–83.
Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Gender differences in chronic pain—findings from a population-based study of Norwegian adults. Pain Manag Nurs. 2004;5:105–17.
Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069.
Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69:719–27.
McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Arch Intern Med. 1993;153:2093–101.
Brim OG, Baltes, PB, Bumpass LL, et al. National survey of midlife development in the United States (MIDUS 1), 1995-1996 [Data file]. Inter-university Consortium for Politcal and Social Research: Ann Arbor, Michigan; 1995–1996 [Cited 22 mar 2018]. Available from: https://doi.org/10.3886/ICPSR02760.v14.
Ryff C, Almeida DM, Ayanian, J, et al. National survey of midlife development in the United States (MIDUS II), 2004-2006 [Data file]. Inter-university Consortium for Politcal and Social Research: Ann Arbor, Michigan; 2004–2006 [Cited 22 mar 2018]. Available from: https://doi.org/10.3886/ICPSR04652.v7.
Ryff C, Almeida DM, Ayanian J, et al. National survey of midlife development in the United States (MIDUS 3), 2013-2014 [Data file]. Inter-university Consortium for Political and Social Research: Ann Arbor, Michigan, 2013–2014 [Cited 22 mar 2018]. Available from: https://doi.org/10.3886/ICPSR36346.v6.
Brown TT, Partanen J, Chuong L, Villaverde V, Griffin AC, Mendelson A. Discrimination hurts: the effect of discrimination on the development of chronic pain. Soc Sci Med. 2018;204:1–8.
Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap. 1994;23:129–38.
Bjørnnes AK, Rustøen T, Lie I, Watt-Watson J, Leegaard M. Pain characteristics and analgesic intake before and following cardiac surgery. Eur J Cardiovasc Nurs. 2014;15:47–54.
Cowan DT, Wilson-Barnett DJ, Griffiths P, Vaughan DJA, Gondhia A, Allan LG. A randomized, double-blind, placebo-controlled, cross-over pilot study to assess the effects of long-term opioid drug consumption and subsequent abstinence in chronic noncancer pain patients receiving controlled-release morphine. Pain Med. 2005;6:113–21.
Harding G, Schein JR, Nelson WW, Vallow S, Olson WH, Hewitt DJ, et al. Development and validation of a new instrument to evaluate the ease of use of patient-controlled analgesic modalities for postoperative patients. J Med Econ. 2010;13:42–54.
Raichle KA, Osborne TL, Jensen MP, Cardenas D. The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain. 2006;7:179–86.
Williams VS, Smith MY, Fehnel SE. The validity and utility of the BPI interference measures for evaluating the impact of osteoarthritic pain. J Pain Symptom Manag. 2006;31:48–57.
Bradburn NM. The structure of psychological well-being. Oxford, England: Aldine; 1969.
Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19.
Taylor JA. A personality scale of manifest anxiety. J Abnorm Soc Psychol. 1953;48:285–90.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: a developmental perspective on happiness. J Pers Soc Psychol. 1998;75:1333–49.
Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–30.
Bae W, Ik Suh Y, Ryu J, Heo J. Physical activity levels and well-being in older adults. Psychol Rep. 2017;120:192–205.
Barrineau MJ, Zarit SH, King HA, Costanzo ES, Almeida DM. Daily well-being of cancer survivors: the role of somatic amplification. Psychooncology. 2014;23:1027–33.
Prenda KM, Lachman ME. Planning for the future: a life management strategy for increasing control and life satisfaction in adulthood. Psychol Aging. 2001;16:206–16.
Diener E, Inglehart R, Tay L. Theory and validity of life satisfaction scales. Soc Indic Res. 2013;112:497–527.
Lucas RE, Donnellan MB. Estimating the reliability of single-item life satisfaction measures: results from four national panel studies. Soc Indic Res. 2012;105:323–31.
McIntosh CN. Report on the construct validity of the temporal satisfaction with life scale. Soc Indic Res. 2001;54:37–56.
Lucas RE, Diener E, Suh E. Discriminant validity of well-being measures. J Pers Soc Psychol. 1996;71:616–28.
Diener E, Chan MY. Happy people live longer: subjective well-being contributes to health and longevity. Appl Psychol Health Well Being. 2011;3:1–43.
Brim OG, Ryff CD, Kessler RC. How healthy are we? A national study of well-being in midlife. Chicago, IL: University of Chicago Press; 2004.
Busseri MA. Toward a resolution of the tripartite structure of hedonic well-being. J Pers. 2015;83:413–28.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-3. Washington, DC: American Psychiatric Association; 1987.
World Health Organization. Composite international diagnostic interview, CIDI, version 10. Geneva, Switzerland: World Health Organization; 1990.
Wittchen HU. Reliability and validity studies of the WHO-composite international diagnostic interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84.
Aalto-Setälä T, Haarasilta L, Marttunen M, Tuulio-Henriksson A, Poikolainen K, Aro H, et al. Major depressive episode among young adults: CIDI-SF versus SCAN consensus diagnoses. Psychol Med. 2002;32:1309–14.
Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization composite international diagnostic interview short-form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7:171–85.
Karlson CW, Gallagher MW, Olson CA, Hamilton NA. Insomnia symptoms and well-being: longitudinal follow-up. Health Psychol. 2013;32:311–9.
Benyamini Y, Leventhal EA, Leventhal H. Self-assessments of health: what do people know that predicts their mortality? Res Aging. 1999;21:477–500.
Little TD. Longitudinal structural equation modeling. New York City: Guilford Press; 2013.
Widaman KF, Thompson JS. On specifying the null model for incremental fit indices in structural equation modeling. Psychol Methods. 2003;8:16–37.
Kline RB. Software review: software programs for structural equation modeling: Amos, EQS, and LISREL. J Psychoeduc Assess. 1998;16:343–64.
MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130–49.
Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles: Muthén & Muthén; 2017.
Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002;9:233–55.
Huta V, Ryan RM. Pursuing pleasure or virtue: the differential and overlapping well-being benefits of hedonic and eudaimonic motives. J Happiness Stud. 2010;11:735–62.
McMahan EA, Estes D. Hedonic versus eudaimonic conceptions of well-being: evidence of differential associations with self-reported well-being. Soc Indic Res. 2011;103:93–108.
Pavot W, Diener E. The affective and cognitive context of self-reported measures of hedonic well-being. Soc Indic Res. 1993;28:1–20.
Vlaeyen JW, Morley S, Crombez G. The experimental analysis of the interruptive, interfering, and identity-distorting effects of chronic pain. Beh Res Ther. 2016;86:23–34.
Seligman ME, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5–14.
Magyar-Moe JL, Owens RL, Conoley CW. Positive psychological interventions in counseling: what every counseling psychologist should know. J Couns Psychol. 2015;43:508–57.
Smith EJ. The strength-based counseling model. Couns Psychol. 2006;34:13–79.
Wong YJ. Strength-centered therapy: a social constructionist, virtues-based psychotherapy. Psychotherapy (Chic). 2006;43:133–46.
Frisch MB. Quality of life therapy: applying a life satisfaction approach to positive psychology and cognitive therapy. New York: John Wiley & Sons Ltd; 2006.
Ruini C, Fava GA. Clinical applications of well-being therapy. In: Linley PA, Joseph S, editors. Positive psychology in practice. Hoboken: John Wiley & Sons Inc; 2004. p. 371–87.
Lopez SJ, Floyd RK, Ulven JC, Snyder CR. Hope therapy: helping clients build a house of hope. In: Snyder CR, editor. Handbook of hope: theory, measures, and applications. San Diego: Academic Press; 2000. p. 123–50.
Rashid T, Anjum A. Positive psychotherapy for young adults and children. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York City: Guilford Press; 2008. p. 250–87.
Müller R, Gertz KJ, Molton IR, Terrill AL, Bombardier CH, Ehde DM, et al. Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and a physical disability. Clin J Pain. 2016;32:32–44.
Peters ML, Smeets E, Feijge M, van Breukelen G, Andersson G, Buhrman M, et al. Happy despite pain: a randomized controlled trial of an 8-week internet-delivered positive psychology intervention for enhancing well-being in patients with chronic pain. Clin J Pain. 2017;33:962–75.
Hausmann LR, Youk A, Kwoh CK, Gallagher RM, Weiner DK, Vina ER, et al. Effect of a positive psychological intervention on pain and functional difficulty among adults with osteoarthritis: a randomized clinical trial. JAMA Netw Open. 2018;1:e182533.
Hausmann LR, Youk A, Kwoh CK, Ibrahim SA, Hannon MJ, Weiner DK, et al. Testing a positive psychological intervention for osteoarthritis. Pain Med. 2017;18:1908–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study received ethical approval from the Institutional Review Board at the University of Wisconsin-Madison.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Kim, S.Y., Shigemoto, Y. & Neduvelil, A. Survive or Thrive? Longitudinal Relation Between Chronic Pain and Well-Being. Int.J. Behav. Med. 26, 486–498 (2019). https://doi.org/10.1007/s12529-019-09805-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-019-09805-3